A Strict Vegetarian Diet May Cause B12 Deficiency
Vitamin B12 and vegetarian diets
Carol L Zeuschner, Bevan D Hokin, Kate A Marsh, Angela V Saunders, Michelle A Reid and Melinda R Ramsay
Med J Aust 2013; 199 (4): S27-S32. || doi: 10.5694/mja11.11509
Published online: 29 October 2013
This is a republished version of an article previously published in MJA Open
Vitamin B12 (cobalamin) is an essential vitamin, required for DNA synthesis (and ultimately cell division) and for maintaining nerve myelin integrity.1 It is found almost exclusively in animal-based products including red meats, poultry, seafood, milk, cheese and eggs. As vitamin B12 is produced by bacteria in the large intestines of animals, plant-based foods are generally not a source of vitamin B12. It is therefore a nutrient of concern for vegetarians and particularly for vegans who choose an entirely plant-based diet. A cross-sectional analysis study involving 689 men found that more than half of vegans and 7% of vegetarians were deficient in vitamin B12.2
Vitamin B12 deficiency
Vitamin B12 deficiency is a serious health problem that can result in megaloblastic anaemia, inhibition of cell division, and neurological disorders.3 Folate deficiency can also cause megaloblastic anaemia and, although a high folate intake may correct anaemia from a vitamin B12 deficiency, subtle neurological symptoms driven by the vitamin B12 deficiency may arise. Loss of intrinsic factor, gastric acid or other protein-digesting enzymes contributes to 95% of known cases of vitamin B12 deficiency.4 Other factors that may contribute to vitamin B12 deficiency are listed in Box 1.13 However, in vegetarian and vegan populations, dietary insufficiency is the major cause.4 Furthermore, high levels of folate can mask vitamin B12 deficiency — a concern for vegetarians and vegans whose folate intake is generally high while vitamin B12 intake is low. The addition of vitamin B12 to any foods fortified with folate has been advocated to prevent masking of haematological and neurological manifestations of vitamin B12 deficiency.14 Subtle neurological damage (even in the absence of anaemia) may be more likely in vegans because of their increased folate levels preventing early detection of vitamin B12 deficiency.4
Vitamin B12 deficiency can also lead to demyelinisation of peripheral nerves, the spinal cord, cranial nerves and the brain, resulting in nerve damage and neuropsychiatric abnormalities. Neurological symptoms of vitamin B12 deficiency include numbness and tingling of the hands and feet, decreased sensation, difficulties walking, loss of bowel and bladder control, memory loss, dementia, depression, general weakness and psychosis.3,4 Unless detected and treated early, these symptoms can be irreversible.
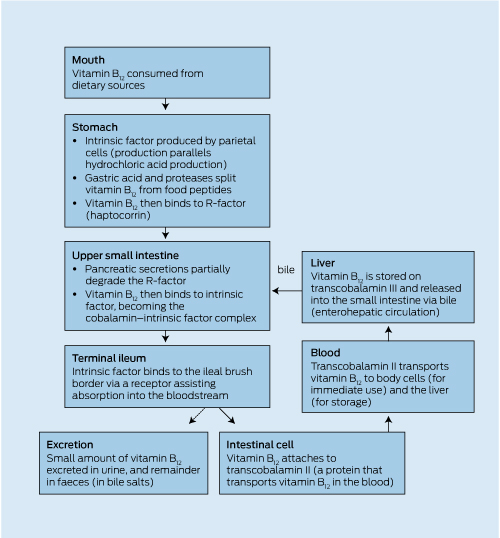
Digestion and absorption of vitamin B12
The digestion of vitamin B12 begins in the stomach, where gastric secretions and proteases split vitamin B12 from peptides. Vitamin B12 is then free to bind to R-factor found in saliva. Pancreatic secretions partially degrade the R-factor, and vitamin B12 is then bound to intrinsic factor. Intrinsic factor binds to the ileal brush border and facilitates the absorption of vitamin B12.15 Box 2 illustrates the process of vitamin B12 digestion and absorption. Vitamin B12 absorption may decrease if intrinsic factor production decreases. There are many well documented factors causing protein-bound vitamin B12 malabsorption, including gastric resection, atrophic gastritis, and the use of medications that suppress acid secretion (see Box 1).
Up to 89% of vitamin B12 consumed in the diet is absorbed, although as little as 9% is absorbed from some foods (including eggs).17,18 This relatively high rate of absorption, combined with low daily requirements and the body's extremely efficient enterohepatic circulation of vitamin B12, contributes to the long period, often years, for a deficiency to become evident. Studies have been inconsistent in linking the duration of following an unsupplemented vegan diet with low serum levels of vitamin B12.2,19 Intestinal absorption is estimated to be saturated at about 1.5–2.0 µg per meal, and bioavailability significantly decreases as intake increases.18
Ageing causes a decreased level of proteases, as well as a reduced level of acid in the stomach. As a result, vitamin B12 is less effectively removed from the food proteins to which it is attached, and food-bound vitamin B12 absorption is diminished.4 The Framingham Offspring Study found that the vitamin B12 from supplements and fortified foods may be more efficiently absorbed than that from meat, fish and poultry.20
While low vitamin B12 status in vegetarians and vegans is predominantly due to inadequate intake, some cases of pernicious anaemia are attributable to inadequate production of intrinsic factor. Under the law of mass action, about 1% of vitamin B12 from large oral doses can be absorbed across the intestinal wall, even in the absence of adequate intrinsic factor.21
Assessing vitamin B12 status
Taking a simple diet history can be a useful indicator of vitamin B12 intake and adequacy. However, laboratory analyses provide a much more accurate assessment. Measurement of serum vitamin B12 levels is a common and low-cost method of assessing vitamin B12 status. The earlier method of measuring vitamin B12 using biological assays was unreliable, as both the active and inactive analogues of vitamin B12 were detected, so levels were often overestimated.17 Modern radio isotope and immunoassay methods reliably measure biologically available analogues of vitamin B12. The early measured ranges of acceptable levels of serum vitamin B12 were determined using individuals who were apparently healthy but had potentially marginal levels of vitamin B12. This has resulted in reference intervals probably being set too low to provide a reliable clinical decision. To improve the ability to predict marginal vitamin B12 status, a higher reference interval (> 360 pmol/L) has been proposed.4,22 Objective measures of neurological damage have been found in patients with vitamin B12 levels below 258 pmol/L.23 However, the usual reference interval for vitamin B12 deficiency is < 220 pmol/L. Achieving national and international agreement on the definition of serum vitamin B12 deficiency would provide some clarity for comparison of studies and reduce variability in defining those at risk of deficiency. Internationally, the cut-off for vitamin B12 varies markedly between < 130 pmol/L and < 258 pmol/L.
Serum vitamin B12 levels alone do not provide a measure of a person's reserves of the vitamin. It is recommended that a metabolic marker of vitamin B12 reserves, such as serum homocysteine, also be determined. Elevated homocysteine levels can be a useful indicator for vitamin B12 deficiency, because serum homocysteine levels increase as vitamin B12 stores fall. While serum homocysteine levels greater than 9 µmol/L suggest the beginning of depleted vitamin B12 reserves,24 standard laboratory reference intervals suggest levels greater than 15 µ mol/L as a marker for depleted vitamin B12 reserves. Although homocysteine levels may also increase with folate or vitamin B6 deficiency, these deficiencies are likely to be rare in vegetarians and vegans.
Other markers for vitamin B12 deficiency include serum holotranscobalamin II (TC2) and urinary or serum methylmalonic acid (MMA). TC2 is the protein that transports vitamin B12 in blood, and its levels fall in vitamin B12 deficiency. Testing for this carrier protein can identify low vitamin B12 status before total serum vitamin B12 levels drop.25 Vitamin B12 is the only coenzyme required in the conversion of methylmalonyl-CoA to succinyl-CoA, so methylmalonyl-CoA levels increase with vitamin B12 deficiency. As it is toxic, methylmalonyl-CoA is converted to MMA, which accumulates in the blood and is excreted in the urine, enabling either urinary or serum MMA to be a useful measure of vitamin B12 reserves. Because TC2 is one of the earliest markers of vitamin B12 deficiency, it may be one of the better means of assessing vitamin B12 status.22
Requirements
Box 3 shows the vitamin B12 nutrient reference values for Australia and New Zealand.26 As no recommended dietary intakes (RDIs) are available for infants under 12 months of age, an adequate intake is recommended instead. Vegans at all stages of the life cycle need to ensure an adequate and reliable source of vitamin B12 from fortified foods, or they will require supplementation equivalent to the RDI.
Vegetarians and vitamin B12 status
While reported cases of frank vitamin B12 deficiency in vegetarians or vegans are rare, several studies have found lower vitamin B12 levels in vegans and vegetarians compared with the general population.27,28 The European Prospective Investigation into Cancer and Nutrition (EPIC)-Oxford cohort study found that 121 of 232 vegans (52%), 16 of 231 vegetarians (7%) and one of 226 omnivores (0.4%) were classed as vitamin B12-deficient.2 There was no significant association between age or duration of subjects' adherence to a vegetarian or vegan diet and the serum levels of vitamin B12.2 Intuitively, it is assumed that prevalence of deficiency increases with a longer duration of vegetarian diet. Although it can take years for deficiency to occur, it is likely that all vegans and anyone who does not regularly consume animal-based foods, and whose diets are unsupplemented or unfortified, will eventually develop vitamin B12 deficiency. Vegetarians and vegans should have their vitamin B12 status regularly assessed to enable early intervention if levels fall too low.
Vegetarian infants and vitamin B12 status
The risk of a breastfed infant becoming deficient in vitamin B12 depends on three factors: the vitamin B12 status of the mother during pregnancy; the vitamin B12 stores of the infant at birth; and the vitamin B12 status of the breastfeeding mother. The fetus obtains its initial store of vitamin B12 via the placenta, with newly absorbed vitamin B12 (rather than maternal stores) being readily transported across the placenta.29 Under normal conditions, full-term infants will have enough stored vitamin B12 at birth to last for about 3 months when the maternal diet does not contain vitamin B12.30 An infant born to a vegetarian or vegan mother is at high risk of deficiency if the mother's vitamin B12 intake is inadequate and her stores are low. Vegetarian women who have repeated pregnancies place infants at greater risk, because their vitamin B12 stores are likely to have been depleted by earlier pregnancies.31 Vegetarian or vegan women must have a balanced diet, including adequate intake of vitamin B12, to provide for their babies during both pregnancy and lactation. Recent studies suggest that maternal stores of vitamin B12 are also reflected in breastmilk. When maternal serum vitamin B12 levels are low, vitamin B12 levels in breastmilk will also be low, and the infant will not receive an adequate vitamin B12 intake.32
There have been reports of deficiency in the breastfed infants of vegan (or "strict vegetarian") mothers who did not supplement their diets with vitamin B12, because of the smaller stores of vitamin B12 gained by the infant during pregnancy and the low vitamin B12 content of breastmilk (reflective of the mothers' serum levels).33,34 Infants have presented with a range of symptoms, often initially signalled by developmental delay.35 Lack of vitamin B12 in the maternal diet during pregnancy has been shown to cause severe retardation of myelination in the nervous system of the infant.36 Visible signs of vitamin B12 deficiency in infants may include involuntary motor movements, dystrophy, weakness, muscular atrophy, loss of tendon reflexes, psychomotor regression, cerebral atrophy, hypotonia and haematological abnormalities.37,38 While supplementation with vitamin B12 results in rapid improvements in laboratory measures of vitamin B12 status, there is continuing research about the long-term effects of deficiency in infants.37
Vitamin B12 in the vegetarian diet
Lacto-ovo-vegetarians will have a reliable source of vitamin B12 in their diet, provided they consume adequate amounts of dairy products and eggs, although their intake is likely to be lower than in meat eaters. However, those who follow a vegan diet will not have a reliable intake unless they consume foods fortified with vitamin B12 or take a supplement.
It was once thought that some plant foods, such as spirulina, and fermented soy products, including tempeh and miso, were dietary sources of vitamin B12, but this has been proven incorrect.39 Recent research has found traces of vitamin B12 in white button mushrooms40 and Korean purple laver (nori),41 but the quantity in a typical serving means that they are not a significant dietary source of this vitamin. An average serving of mushrooms contains about 5% of the RDI, making the quantity required to supply adequate amounts of vitamin B12 to vegetarians impractical. Further, use of Korean laver is unlikely to be widespread in the Australian diet. With the unique exception of these two plant foods,40,41 any vitamin B12 detected in other plant foods is likely to be the inactive analogue, which is of no use to the body and can actually interfere with the absorption of the active form.42
Box 4 shows a sample vegetarian meal plan for a 19–50-year-old woman, which includes food sources typical in a Western-style diet and meets the RDI of vitamin B12 and requirements for other key nutrients (except vitamin D and long-chain omega-3 fatty acids). Excluding or limiting dairy foods or fortified soy milk from the vegetarian diet would necessitate the need for vitamin B12 supplements.
Fortified foods
In contrast to the United States, where foods are extensively fortified with vitamin B12, Food Standards Australia New Zealand permits only a limited number of foods to be fortified with vitamin B12. This includes selected soy milks, yeast spread, and vegetarian meat analogues such as soy-based burgers and sausages. Examples of the vitamin B12 content of foods suitable for vegetarians are shown in Box 5.
Vitamin B12 added to foods is highly bioavailable, especially in people with vitamin B12 deficiency caused by inadequate dietary intake. An unpublished Australian study (Hokin BD. Vitamin B12 deficiency issues in selected at-risk populations [PhD thesis]. Newcastle: University of Newcastle, 2003) compared the effectiveness of fortified soy milk (two servings of 250 mL/day), soy-based meat analogues (one serving/day), vitamin B12 supplements (one low-dose tablet/day or one high-dose tablet/week) and vitamin B12 intramuscular injections (one injection/month) in raising serum vitamin B12 levels in subjects with deficiency. The study found that fortified foods were superior to the traditional methods of supplementation (intramuscular injections and tablets). Further research would be beneficial to confirm these findings. With inadequate dietary intake being a risk for vegetarians and vegans, further fortification of foods commonly consumed by this population with vitamin B12 would be beneficial and should be considered by the relevant authorities.
Supplements
In a vegan diet, using a supplement or consuming fortified foods is the only way to obtain vitamin B12. As the body can only absorb a limited amount of vitamin B12 at any one time, it is better to take small doses more often, instead of large doses less often. One study found that small doses of vitamin B12 in the range of 0.1–0.5 µg resulted in absorption ranging between 52% and 97%; doses of 1 µg and 5 µg resulted in mean absorption of 56% and 28%, respectively, while higher doses had even lower absorption, with 10 µg and 50 µg doses resulting in 16% and 3%, respectively, being absorbed.17 While sublingual supplements are often promoted as being more efficiently absorbed, there is no evidence to show that this form of supplement is superior to regular oral vitamin B12.44 Vitamin B12 supplements are not made from animal-based products and are suitable for inclusion in a vegan diet.
Conclusion
Vitamin B12 deficiency is a potential concern for anyone with insufficient dietary intake of vitamin B12, including those adhering to a vegan or vegetarian diet or significantly restricting animal-based foods. Studies have found that vegetarians, particularly vegans, have lower serum vitamin B12 levels, and it is likely that anyone avoiding animal-based foods will eventually become deficient if their diet is not supplemented. All vegans, and lacto-ovo-vegetarians who don't consume adequate amounts of dairy products or eggs to provide sufficient vitamin B12, should therefore supplement their diet with vitamin B12 from fortified foods or supplements. It is particularly important that pregnant or breastfeeding vegan and vegetarian women consume a reliable source of vitamin B12 to reduce the risk of their baby developing a vitamin B12 deficiency.
1 Causes of vitamin B12 deficiency, with contributing factors
Inadequate dietary intake
-
Restrictive diet or dieting; vegetarian or vegan diets without supplementation or use of fortified foods
Inadequate absorption or impaired utilisation
-
Loss of intrinsic factor, loss of gastric acid and/or other protein-digesting enzymes (contributes to 95% of known cases)4
-
Use of medications that suppress acid secretion, including somatostatin, cholecystokinin, atrial natriuretic peptide, and nitric oxide5
-
Pancreatic disease
-
Gastric resection, sleeve or banding surgery6
-
Ileal disease or ileal resection (secondary to Crohn's disease)7
-
Use of metformin (oral hypoglycaemic agent)6
-
Use of angiotensin-converting enzyme inhibitor9
-
Use of levodopa and catechol-O-methyltransferase inhibitors10
-
Autoimmunity to intrinsic factor
-
Gastric infection with Helicobacter pylori11
-
Ileocystoplasty12
-
Atrophic gastritis
Increased requirements
-
During pregnancy and lactation
Increased excretion
-
Alcoholism
2 Diagram illustrating vitamin B12 digestion and absorption15,16
3 Recommended dietary intake (RDI)* and estimated average requirement (EAR)† of vitamin B12 per day26
| Sex and age group | RDI | EAR | |||||||||||||
| | |||||||||||||||
| Men = 19 years | 2.4 µg | 2.0 µg | |||||||||||||
| Women = 19 years | 2.4 µg | 2.0 µg | |||||||||||||
| Pregnant women | 2.6 µg | 2.2 µg | |||||||||||||
| Lactating women | 2.8 µg | 2.4 µg | |||||||||||||
| Children | |||||||||||||||
| 0–6 months | 0.4 µg‡ | ||||||||||||||
| 7–12 months | 0.5 µg‡ | ||||||||||||||
| 1–3 years | 0.9 µg | 0.7 µg | |||||||||||||
| 4–8 years | 1.2 µg | 1.0 µg | |||||||||||||
| 9–13 years | 1.8 µg | 1.5 µg | |||||||||||||
| 14–18 years | 2.4 µg | 2.0 µg | |||||||||||||
| | |||||||||||||||
| * The RDI is the average daily dietary intake level that is sufficient to meet the nutrient requirements of nearly all healthy individuals (97%–98%) of a particular sex and life stage. † The EAR is a daily nutrient level estimated to meet the requirements of half the healthy individuals of a particular sex and life stage. ‡ These values are adequate intakes, which are the average daily nutrient intake levels based on observed or experimentally determined approximations or estimates of nutrient intake by a group (or groups) of apparently healthy people that are assumed to be adequate. | |||||||||||||||
4 A sample vegetarian meal plan designed to meet requirements for vitamin B12 and other key nutrients for a 19–50-year-old woman, showing vitamin B12 content of the foods*
| Meal | Vitamin B12 content | ||||||||||||||
| | |||||||||||||||
| Breakfast | |||||||||||||||
| Bowl of cereal with fruit, and poached egg on toast | |||||||||||||||
| 2 wholegrain wheat biscuits | 0.0 µg | ||||||||||||||
| 4 strawberries | 0.0 µ g | ||||||||||||||
| 10 g chia seeds | 0.0 µg | ||||||||||||||
| 1/2 cup low-fat fortified soy milk (or dairy milk) | 0.5 µ g (0.8 µ g)† | ||||||||||||||
| 1 slice multigrain toast | 0.0 µ g | ||||||||||||||
| 1 poached egg | 0.9 µg | ||||||||||||||
| Snack | |||||||||||||||
| Nuts and dried fruit | |||||||||||||||
| 30 g cashews | 0.0 µ g | ||||||||||||||
| 6 dried apricot halves | 0.0 µg | ||||||||||||||
| Lunch | |||||||||||||||
| Chickpea falafel wrap | |||||||||||||||
| 1 wholemeal pita flatbread | 0.0 µ g | ||||||||||||||
| 1 chickpea falafel | 0.0 µ g | ||||||||||||||
| 30 g hummus | 0.0 µ g | ||||||||||||||
| 1/2 cup tabouli | 0.0 µ g | ||||||||||||||
| Salad | 0.0 µ g | ||||||||||||||
| Snack | |||||||||||||||
| Banana and wheatgerm smoothie | |||||||||||||||
| 3/4 cup low-fat fortified soy milk (or dairy milk) | 0.8 µ g (1.1 µ g)† | ||||||||||||||
| 2 teaspoons wheatgerm | 0.0 µ g | ||||||||||||||
| 1 banana | 0.0 µ g | ||||||||||||||
| Dinner | |||||||||||||||
| Stir-fry greens with tofu and rice | |||||||||||||||
| 100 g tofu | 0.0 µg | ||||||||||||||
| 2 spears asparagus, 1/3 cup bok choy and 25 g snow peas | 0.0 µ g | ||||||||||||||
| 1 cup cooked brown rice | 0.0 µ g | ||||||||||||||
| Snack | |||||||||||||||
| Fortified malted chocolate beverage | |||||||||||||||
| 1 cup low-fat fortified soy milk (or dairy milk) | 1.0 µ g (1.5 µ g)† | ||||||||||||||
| 10 g malted chocolate powder | 0.0 µ g | ||||||||||||||
| Total vitamin B 12 | 3.2 µ g (4.3 µ g) † | ||||||||||||||
| | |||||||||||||||
| * Source: FoodWorks 2009 (incorporating Food Standards Australia New Zealand's AUSNUT [Australian Food and Nutrient Database] 1999), Xyris Software, Brisbane, Qld. † Figures are for soy milk (dairy milk). | |||||||||||||||
5 Vitamin B12 content of lacto-ovo-vegetarian food sources*
| Vegetarian sources | Vitamin B12 per 100 g | ||||||||||||||
| | |||||||||||||||
| Sausage, vegetarian style, fortified | 2.0 µ g | ||||||||||||||
| Cheese, cheddar, reduced fat (16%) | 1.8 µg | ||||||||||||||
| Egg (chicken), whole, poached | 1.7 µ g | ||||||||||||||
| Milk, cow, fluid, regular or reduced fat | 0.6 µ g | ||||||||||||||
| Soy beverage, unflavoured, regular fat, fortified | 0.9 µ g | ||||||||||||||
| Soy beverage, unflavoured, reduced fat (1.5%), fortified | 0.9 µ g | ||||||||||||||
| Soy beverage, unflavoured, low fat, (0.5%), fortified | 0.3 µ g | ||||||||||||||
| Yoghurt dessert, regular fat, flavoured | 0.2 µg | ||||||||||||||
| | |||||||||||||||
| * From Food Standards Australia New Zealand. NUTTAB 2010 online searchable database.43 | |||||||||||||||
Provenance: Commissioned by supplement editors; externally peer reviewed.
A Strict Vegetarian Diet May Cause B12 Deficiency
Source: https://www.mja.com.au/journal/2013/199/4/vitamin-b12-and-vegetarian-diets
0 Response to "A Strict Vegetarian Diet May Cause B12 Deficiency"
Post a Comment